Cardiomyopathy
Also known as: Heart muscle disease
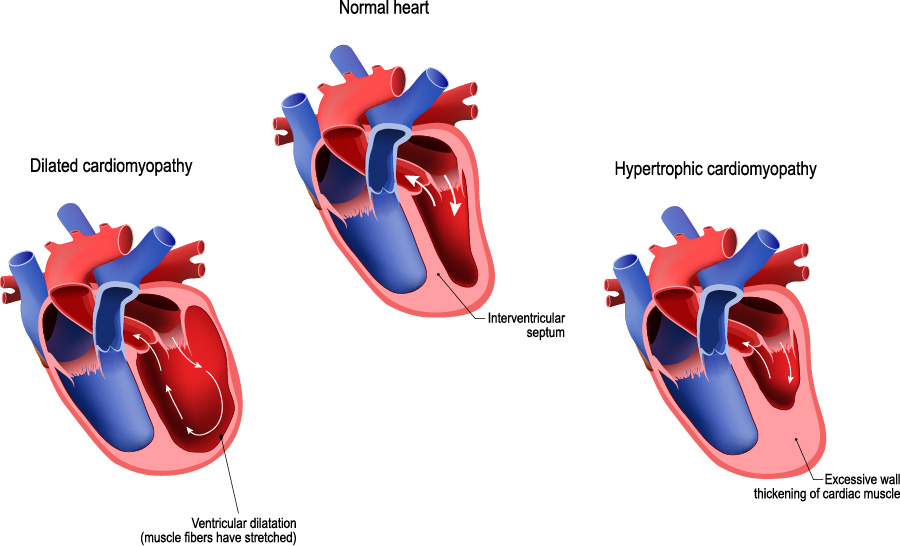
The normal heart muscle carries out the pumping action by squeezing and relaxing in a rhythmic way.
Cardiomyopathy is a condition that causes the heart muscle either to stretch, stiffen, or thicken, causing the heart to not pump properly. As this progresses, it can ultimately lead to heart failure.
Ischemic Cardiomyopathy:
Due to damage caused by coronary artery disease and heart attacks causing decreased blood flow to the heart.
Nonischemic Cardiomyopathy:
Dilated Cardiomyopathy – caused by overstretching of the heart. Due to this, the heart can’t squeeze blood out properly.
Causes:
- Valvular disease
- Heavy alcohol use
- Vitamin B1 (Thiamine) deficiency
- Thyroid imbalances
- Infections
- Complications during or after pregnancy
- Diabetes
- Obesity
- Kidney Disease
- Long History of High Blood Pressure
- Prolonged Tachycardia (high heart rate)
- Medications – certain chemotherapy agents
- Illicit drugs – like steroids, cocaine, amphetamines
- Family history
- Unknown
Hypertrophic Cardiomyopathy – occurs when the heart muscle becomes too thick, especially the left ventricle and the septum (the muscle that divides left and right ventricles). This reduces the amount of blood the heart can squeeze out. If the septum becomes thick enough that it blocks the blood from going out of the heart, it is called Hypertrophic Obstructive Cardiomyopathy (HOCM). This may cause sudden death, especially in athletes.
Causes:
- Family history
- High blood pressure
- Old age
- Unknown
Restrictive Cardiomyopathy – occurs when the heart muscle becomes too stiff. After the heart squeezes out blood, it can’t relax properly so the blood can’t properly fill the heart before it pumps again.
Causes:
- Scarring of heart muscle
- Iron building up in the heart (hemochromatosis)
- Cancer medication
- Radiation
- Other systemic diseases like sarcoidosis
- Amyloidosis
- Unknown
Arrhythmogenic Right Ventricular Dysplasia – a rare, genetic type that occurs when scar tissue replaces the healthy muscle of the right ventricle
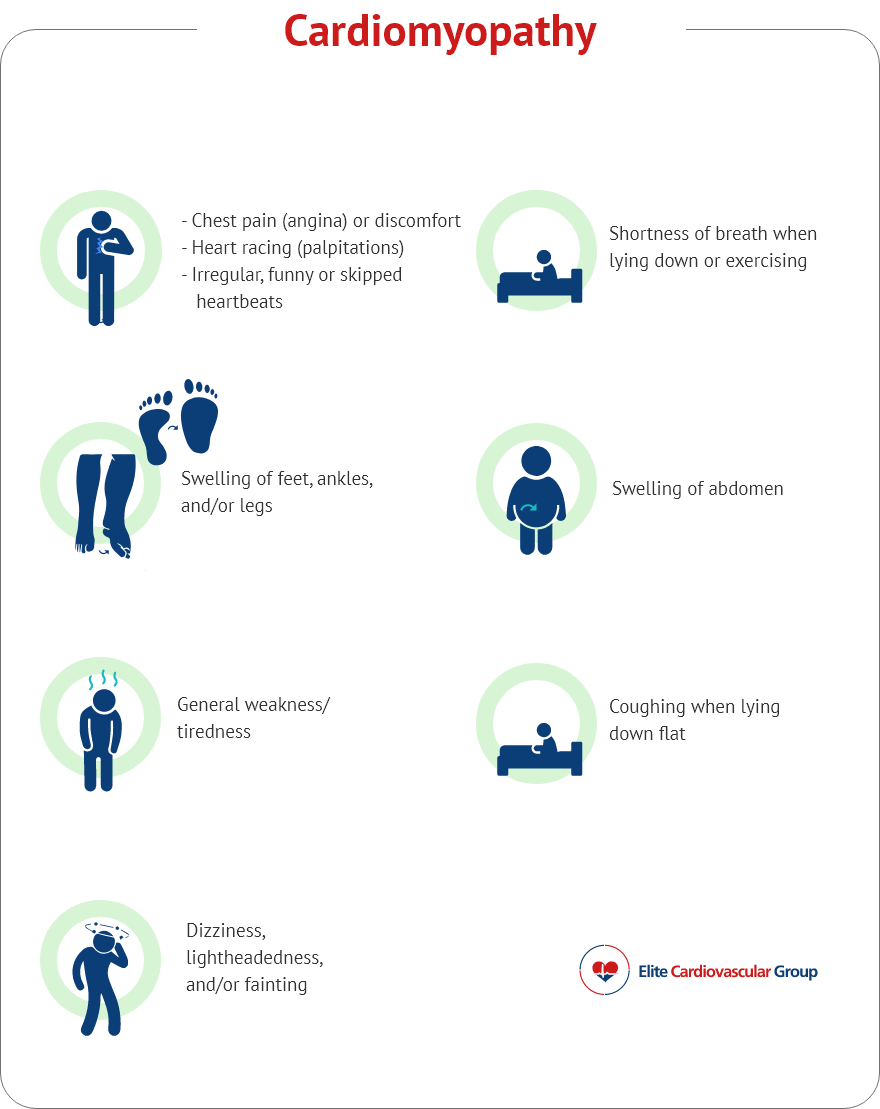
Note: Not everyone may experience all symptoms
Show references
Ommen SR, et al. Hypertrophic cardiomyopathy—one case per year? a clarion call to do what is right. JAMA Cardiology. 2016;1(3):333-334.
Marian AJ, Braunwald E. Hypertrophic Cardiomyopathy: Genetics, Pathogenesis, Clinical Manifestations, Diagnosis, and Therapy. Circ Res. 2017;121(7):749-770. doi:10.1161/CIRCRESAHA.117.311059
Rammos A, Meladinis V, Vovas G, Patsouras D. Restrictive Cardiomyopathies: The Importance of Noninvasive Cardiac Imaging Modalities in Diagnosis and Treatment-A Systematic Review. Radiol Res Pract. 2017;2017:2874902. doi:10.1155/2017/2874902
Rizzo S, Carturan E, De Gaspari M, Pilichou K, Thiene G, Basso C. Update on cardiomyopathies and sudden cardiac death. Forensic Sci Res. 2019;4(3):202-210. Published 2019 Aug 19. doi:10.1080/20961790.2019.1631957
Sisakian H. Cardiomyopathies: Evolution of pathogenesis concepts and potential for new therapies. World J Cardiol. 2014;6(6):478-494. doi:10.4330/wjc.v6.i6.478
Schultheiss HP, Fairweather D, Caforio ALP, et al. Dilated cardiomyopathy. Nat Rev Dis Primers. 2019;5(1):32. Published 2019 May 9. doi:10.1038/s41572-019-0084-1
Bhandari B, Quintanilla Rodriguez BS, Masood W. Ischemic Cardiomyopathy. [Updated 2020 Sep 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537301/
